Diabetes is a chronic (long-term) condition that impacts how your body gets energy from the foods you eat, according to the CDC. Knowing the difference between type 1 and type 2 diabetes is important because each type has unique causes, risk factors, treatment options, and management techniques.
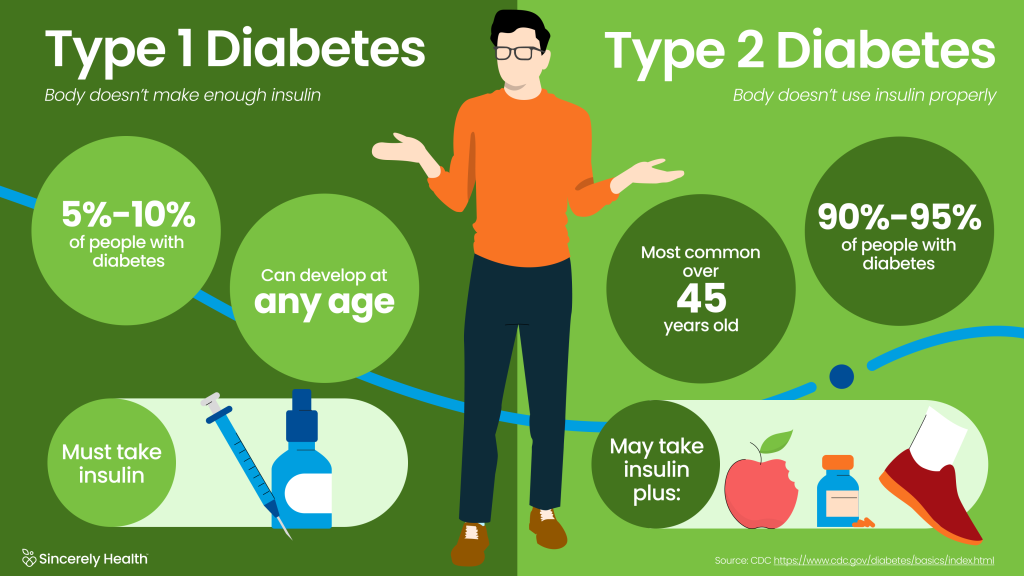
For Type 1 diabetes, the body doesn’t make enough insulin. About 5 to 10% of people with diabetes have Type 1. Type 1 can develop at any age, and the person must take insulin. For Type 2 Diabetes, the body doesn’t use insulin properly. Type 2 is most common over 45 years old, 90-95% of people with diabetes have Type 2, and they may take insulin or manage with food choices, medication, and exercise.
What is diabetes?
Your body needs energy to work and stay healthy, and it gets most of that energy from breaking down food into glucose (sugar).
When glucose enters your bloodstream, it raises your blood sugar. This tells your pancreas that it’s time to release some insulin. As the insulin travels through your body, it acts like a key, letting the glucose into your cells, where it’s converted into energy.
In people with diabetes, there’s a gap between how much insulin you need and how much your body can make, leading to high blood sugar. In type 1 diabetes, the pancreas doesn’t make insulin at all. In type 2 diabetes and gestational diabetes, the body still makes insulin, but it either doesn’t make enough or doesn’t use it very well.
Type 1 Diabetes
About 5 to 10% of people with diabetes have Type 1 diabetes.
In type 1 diabetes, an autoimmune reaction causes the body’s immune system to attack healthy insulin-producing cells in the pancreas. Over time, this destroys the body’s ability to make insulin.
Type 1 diabetes can develop at any age, but it most commonly occurs in children, teens, and young adults. You may be more likely to develop type 1 diabetes if you have a parent or sibling with the condition. At this time, there’s no known way to prevent type 1 diabetes.
Symptoms of type 1 diabetes can appear suddenly over several days or weeks and may include being more hungry or thirsty than usual, frequent urination, blurry vision, fatigue, and weight loss.
Type 1 diabetes is diagnosed with blood tests to measure blood glucose. Treatment usually involves multiple daily insulin injections and self-monitoring blood sugar.
Type 2 Diabetes
About 90-95% of people with diabetes have Type 2 diabetes.
It happens when your body doesn’t make enough insulin (insulin deficiency) or your cells don’t react to it very well (insulin resistance), leading to high blood sugar.
Type 2 diabetes can develop at any age, but it’s usually diagnosed in adults who are middle-aged or older. Risk factors include:
- Family history of diabetes
- Lifestyle factors (age, weight, diet, physical activity level)
You may help prevent type 2 diabetes by eating nutrient-rich foods, reaching and maintaining a healthy weight, and exercising regularly.
Symptoms of type 2 diabetes can develop slowly over several years and include being more hungry or thirsty than usual, frequent urination, blurry vision, fatigue, and weight loss.
Type 2 diabetes is diagnosed with blood tests to measure blood glucose. Treatment usually involves healthy lifestyle changes, sometimes accompanied by medication and insulin.
Gestational Diabetes
Gestational diabetes is a type of diabetes that only develops during pregnancy, usually diagnosed between weeks 24 and 28. Most of the time, blood sugar levels can be managed by eating healthy and exercising regularly, but sometimes insulin is also needed.
Symptoms and Complications of Type 1 and Type 2 Diabetes
People with either type of diabetes may experience symptoms and complications linked to high blood sugar, including:
- Dry mouth
- Feeling very thirsty
- Feeling very hungry, even after eating
- Urinating often
- Blurry vision
- Feeling tired or weak
- Losing weight without trying
- Tingling or numbness in the hands and feet
- Sores that won’t heal
Some diabetes complications can be sudden and severe, and they require emergency treatment. These include:
- Diabetes-related ketoacidosis (DKA): A life-threatening diabetes complication where a lack of insulin causes the body to make too much of a chemical called ketones, which can turn blood acidic.
- Hyperosmolar hyperglycemic state (HHS): A serious complication that happens when blood sugar levels are too high for too long. HHS leads to severe dehydration, confusion, and other life-threatening complications.
- Hypoglycemia: Also known as extremely low blood sugar, severe hypoglycemia can lead to seizures, loss of consciousness, and even death if left untreated.
Long-term complications of type 1 and type 2 diabetes may include:
- Heart disease, heart attack, and stroke
- Eye damage that can lead to blindness
- Nerve damage that causes tingling, numbness, or pain
- Kidney disease
- Foot problems
- Oral health issues
Managing Type 1 and Type 2 Diabetes
Managing type 1 and type 2 diabetes involves:
- Self-monitoring blood sugar levels: Don’t forget to record your measurements! They’re a great tool for making informed decisions about your diet, physical activity, and treatment.
- Regular checkups: Here, you’ll set goals to help manage your condition , often by measuring 3 key things—A1C (your average blood sugar over the last 3 months), blood pressure, and cholesterol. Just think ABCs!
- Meal planning: A diabetes meal plan should include a balance of nutritious foods from all food groups, prioritizing sources of fiber, heart-healthy protein, and healthy fats. Try to avoid saturated and trans fats, high-salt (sodium) foods, and high-sugar foods.
- Physical activity: Regular exercise can help improve heart health, blood pressure, muscle strength, and insulin sensitivity. In people with type 2 diabetes, it may also help lower blood glucose and promote healthy weight loss.
- Finding your community: Supportive resources and community can be a real source of strength when living with diabetes. If you don’t know where to start, check out the American Diabetes Association’s Tools and Resources page and database of diabetes organizations and events.



















